Cornerstone
TRICARE SUBSTANCE ABUSE TREATMENT
Learn about TriCare drug rehab coverage and get help at our Arizona rehab centers that accept TriCare's policies
TRICARE DRUG TREATMENT COVERAGE
Starting the journey toward recovery requires exploring the available treatment options, and TriCare’s drug rehab coverage is instrumental in connecting individuals with necessary care.
Cornerstone Healing Center is proud to accept TriCare insurance, enabling us to offer comprehensive substance abuse treatment programs to those who need them.
Our commitment to offering personalized and high-quality care involves a combination of evidence-based and holistic therapies that promote healing and long-term recovery.
Let us guide you through the details of TriCare coverage and our various programs. We’ll work together to create a plan that helps you build a healthier future free from substance abuse.
Jump to the following sections
View our addiction treatment locations
Now Accepting AHCCCS Health Choice,
Mercy Care, TriCare, and Triwest
Addictions we treat at Cornerstone
TRICARE COVERED DRUG REHAB PROGRAMS

Our Residential Treatment Programs provide comprehensive and ongoing support for individuals struggling with substance abuse. We offer a combination of detoxification, therapeutic counseling, and holistic healing practices. Our programs employ evidence-based methods such as Cognitive-Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT), incorporating mindfulness exercises, yoga, and nutrition therapy. Our goal is to identify and address the underlying causes of addiction, equipping individuals with the necessary skills to achieve lasting recovery and prevent relapse.

Our Partial Hospitalization Programs (PHP) deliver an all-encompassing and methodical recovery strategy. Operating five days a week, six hours daily, these programs offer rigorous daytime treatment that encompasses therapeutic counseling, group discussions, and holistic activities without needing overnight accommodation. This method aids participants in confronting and managing their addiction, equipping them with crucial skills and support for enduring sobriety. The PHP model strongly emphasizes personal responsibility and motivates participants to utilize their newfound skills in everyday life scenarios.

Our Outpatient Programs are divided into three types: Intensive Outpatient Program (IOP) and the standard Outpatient Program. The IOP is the initial step, while the standard Outpatient Program runs three days a week and has a flexible schedule to accommodate personal commitments and responsibilities. Both Programs offer various therapeutic interventions, including one-on-one counseling, group sessions, and skill-enhancement workshops. Our holistic approach aims to provide a nurturing path to recovery and help restore the lives impacted by addiction.
TriCare Health Insurance
TriCare health insurance is a comprehensive healthcare program that offers a range of medical services to uniformed service members, retirees, and their families worldwide.1 It includes hospitalization, outpatient care, mental health services, and prescription medications. TriCare was established in the late 20th century to replace the Civilian Health and Medical Program of the Uniformed Services (CHAMPUS). It collaborates with military and civilian healthcare networks and offers various plans that suit the unique medical needs of the military community. Its mission is to provide high-quality and accessible healthcare services to support the health and well-being of its members.
ABOUT TRICARE DRUG TREATMENT COVERAGE
TriCare insurance provides an extensive coverage plan for substance abuse treatments. This coverage acknowledges the importance of accessible care for those who struggle with addiction. The coverage plan includes various services, such as detoxification, inpatient and outpatient rehabilitation, therapy, and counseling sessions.2 The substance abuse treatment benefits are designed to support the unique needs of military members, retirees, and their families. The aim is to provide comprehensive care to ensure individuals receive the necessary support for a successful recovery journey. The coverage plan emphasizes the importance of physical and mental health rehabilitation.
Alumni Client Family Testimonial
I feel like Cornerstone gave him all the right tools. He knew how to do it. It was something we could have never done. I just could totally see kind of a personality change in him of wanting, and knowing, that he could achieve and do higher things and greater things. That has to be the people (at Cornerstone).”
Nicole A. - Mother of a Cornerstone Alumni
What Addictions Does TriCare Provide Coverage For?
Addictions Covered by TriCare
TriCare policies extend comprehensive coverage for substance abuse disorders, including treatments for alcohol and drug rehabilitation. Below are some of the addictions our Arizona facilities treat, which are typically included under your TriCare health insurance:
- Alcohol: TriCare insurance supports holistic programs aimed at alcohol addiction recovery.
- Opioids: TriCare offers in-depth care and assistance for individuals addressing opioid addiction.
- Fentanyl: TriCare insurance encompasses treatments for fentanyl addiction with specialized care and support.
- Cocaine: Treatment plans specifically designed to address cocaine dependency and promote long-lasting sobriety are covered by TriCare.
- Methamphetamine: TriCare insurance provides aid for methamphetamine addiction treatment, emphasizing the resolution of fundamental recovery challenges.
- Benzodiazepine: TriCare covers programs focused on benzodiazepine withdrawal and subsequent rehabilitation.
- Co-Occurring Disorders: Tailored therapy for those dealing with both addiction and mental health issues is included in TriCare coverage.
Programs We Offer
Understanding Your TriCare Health Insurance Card
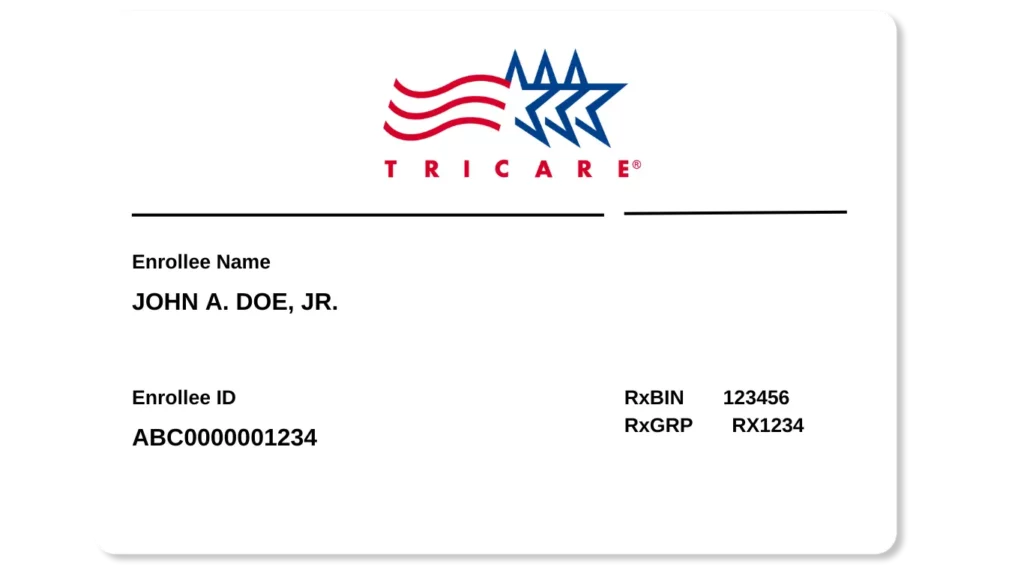
Card Front
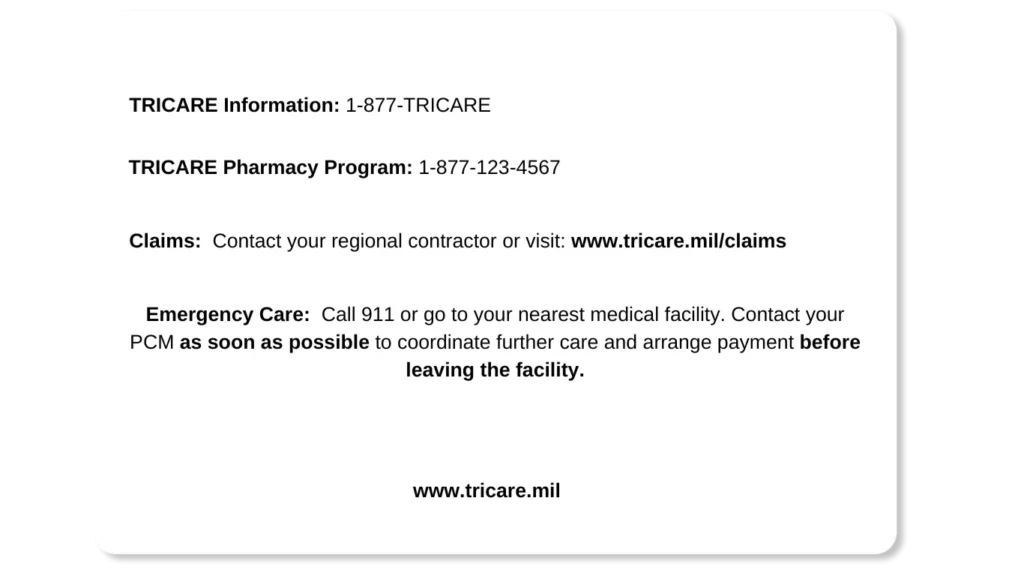
Card Back
Cornerstone's Scottsdale Clinical Team
Clinical Director of Scottsdale Program
Lionel is a Licensed Independent Substance Abuse Counselor (LISAC) with over 4 years at Cornerstone. Passionate about helping those with addiction and mental health struggles, and he has trained as an EMDR therapist, adopting a trauma-informed approach to find and treat underlying root causes with empathy.

Clinical Director of Phoenix Program
Nate began his recovery journey in 2010 and earned a Master’s in Social Work from ASU. He’s been in the Behavioral Health field since 2013. Specializing in CBT, DBT, and grief, Nate is now the Clinical Director of our Phoenix program, underlined by his passion for helping others who struggled with substance abuse issues as he did.
FAQs About TriCare
Get Answers to the most commonly asked questions about TriCare Drug Rehab
What types of drug rehab programs Does TriCare Health cover?
TriCare offers a broad spectrum of coverage to assist individuals confronting substance use disorders, emphasizing both immediate medical intervention and holistic, long-term recovery.
Below is an overview of services TriCare supports:
- Inpatient Services (Including Emergency): TriCare provides coverage for both emergency interventions and planned inpatient care, ensuring timely access to necessary treatments without delay.3
- Intensive Outpatient Programs (IOPs): TriCare supports intensive outpatient programs for individuals requiring regular oversight without the need for constant inpatient care. These programs typically feature group therapy, individual counseling, and structured recovery activities.4
- Detoxification: Recognizing the difficulty of managing withdrawal symptoms, TriCare covers detoxification services, which are crucial for the safe mitigation of withdrawal under professional supervision.
- Mental Health Services: Acknowledging the frequent overlap between addiction and mental health issues, TriCare extends coverage to a variety of mental health services, including cognitive-behavioral therapy (CBT), psychotherapy, and counseling, to tackle underlying mental health challenges.
- Opioid Treatment Programs: For severe opioid dependency, TriCare includes comprehensive treatment programs that combine medication-assisted treatment, counseling, and ongoing recovery planning.
- Partial Hospitalization Programs (PHPs): PHPs balance intensive inpatient care and outpatient services, covered by TriCare, facilitating substantial care without overnight stays.
- Residential Treatment for Substance Use Disorders: TriCare also covers residential treatment programs for individuals needing immersive, 24/7 care. These programs offer medical oversight, therapy, and peer support in a residential setting.
TriCare’s wide-ranging coverage ensures that military members and their families have access to varied treatment pathways, catering to diverse needs for achieving sustainable recovery from substance abuse.
Will TriWest cover my stay in drug rehab?
TriCare is committed to providing comprehensive healthcare assistance, including coverage for medically necessary substance use treatment.
If a healthcare professional determines that your rehabilitation stay is essential for your health and recovery, TriCare typically covers the associated treatment expenses, depending on the specifics of your policy.
However, to fully understand your benefits, you should review your TriCare policy or speak with a Cornerstone admissions representative for detailed coverage information.
We can verify your insurance coverage, check your benefits, and ensure you receive the necessary treatment.
How do I find out what my policy covers?
To determine what your TriCare insurance plan covers, follow these steps:
- Review Your Policy Documentation: Read your TriCare insurance policy documents thoroughly. Look for sections on coverage limits, exclusions, deductibles, and co-pays.5
- Visit the TriCare Website: The official TriCare website provides detailed information about various plans and coverage. Use the site to find specifics related to your policy type.
- Contact TriCare Directly: Contact TriCare customer service for direct inquiries. Have your policy number ready for reference so you can ask specific questions about your coverage.
- Use the TriCare Coverage Tool: Utilize online tools provided by TriCare to check coverage for specific treatments or services. This can give you a clearer understanding of what is included in your plan.
- Consult With Your Healthcare Provider: Healthcare providers often have experience with TriCare billing and can offer insights into what services are typically covered under your plan.
- Check for Pre-Authorization Requirements: Determine if TriCare requires pre-authorization to ensure the services you need are covered.
- Understand In-Network vs. Out-of-Network Services: Know the difference in coverage levels for in-network versus out-of-network providers to avoid unexpected expenses.
- Seek Assistance from a Military Health System Counselor: Military health system counselors or patient advocates can provide guidance and help navigate your TriCare coverage.
- Review Annual Updates: Insurance policies can change, so it’s important to review any updates to your TriCare plan annually or as notifications are received.
Taking these steps can help clarify what your TriCare insurance plan policy covers, ensuring you make the most out of your benefits.
Will TriCare pay for rehab more than once?
Tricare covers addiction treatments, subject to specific policy terms, limitations, exclusions, and medical necessity, including outcomes of past treatments.
To understand your coverage better, here are some important aspects that you should keep in mind:
- Annual and Lifetime Limits: Policies might restrict the number of substance abuse treatment sessions within a year or across the policy’s duration. It’s crucial to check your plan for any specified limits on treatment frequency or covered days.
- Medical Necessity: TriCare generally requires a healthcare professional to confirm the medical necessity for each treatment phase, underscoring the treatment’s importance for recovery.
- Prior Treatment Outcomes: Coverage decisions for additional treatment sessions often consider the success and progress of previous treatments, evaluating the need and potential benefits of ongoing treatment.
- Type of Treatment: The coverage may vary depending on the treatment type; for instance, TriCare might consistently cover outpatient therapy sessions annually more than multiple inpatient rehabilitation stays.
- Policy Specifics: It is essential to familiarize yourself with the details of your specific TriCare policy, as policies manage coverage for repeated treatments in considerable variation.
- Pre-Authorization: Similar to initial treatments, follow-up treatments typically require pre-authorization from TriCare to confirm coverage eligibility and medical necessity.
To better understand your coverage for addiction treatments, review your TriCare policy, get in touch with Cornerstone for insurance verification, or speak directly with a TriCare representative to discuss coverage for ongoing treatment.
Are there any restrictions on types of addiction treatment TriCare will pay for?
Like other insurance providers, TriCare sets certain restrictions or limitations on the addiction treatments it covers, considering factors like medical necessity, evidence-based effectiveness, cost efficiency, and the details of your specific insurance plan.6
Common restrictions may include:
- Type of Treatment: Coverage may be restricted to certain types of treatment, such as inpatient, outpatient, or Medication-Assisted Therapy (MAT). In contrast, more luxurious or experimental treatments might not be covered.
- Provider Network: TriCare has a network of approved addiction treatment providers. Getting care outside this network could lead to higher out-of-pocket costs or lack of coverage.
- Pre-Authorization Requirement: Many TriCare plans require pre-authorization for addiction treatment services, meaning approval is needed in advance to ensure coverage.
- Duration and Frequency of Treatment: Limits may be placed on how long and how often treatments can be received, for example, a maximum number of days for inpatient care or a limited number of therapy sessions.
- Substance-Specific Coverage: The coverage might differ based on the substance being treated, with certain substances or behaviors possibly facing exclusions or limitations.
- Evidence-Based Treatments: TriCare generally covers treatments proven effective through scientific research.
- Appropriate Level of Care: Coverage is provided only for the level of care deemed necessary for the patient’s specific condition, which could restrict access to more intensive treatment options unless there is a medical justification.
There are many factors to consider when determining your coverage.
Contact our admissions team for personalized guidance based on your unique situation.
How soon can I get into rehab with TriCare coverage?
We have made the admission process as simple and convenient as possible.
Once we verify your TriCare insurance, we can proceed with treatment planning and admission without delays.
So you can start your journey toward recovery as soon as possible!
Sources
CLINICALLY REVIEWED
Lionel Estrada, LISAC
CLINICAL DIRECTOR
Lionel, a Licensed Independent Substance Abuse Counselor (LISAC) with over 4 years at Cornerstone, specializes in addiction and mental health. Trained in EMDR therapy, he employs a trauma-informed, empathetic approach to address underlying causes of these issues.
- Read our Editorial Policy
Still have questions about treatment?
Our admissions specialists are here to explain the process, answer any questions you may have, and ensure you’re getting the help you need to live a healthy life free from addiction.






















