Cornerstone
CARELON SUBSTANCE ABUSE TREATMENT
Learn about Carelon drug rehab coverage and get help at our Arizona rehab centers that accept Carelon's plans
CARELON DRUG TREATMENT COVERAGE
Starting on the path to recovery means understanding your options. Getting coverage for drug rehab may be the solution to getting the help you need.
At Cornerstone Healing Center, we are pleased to accept Carelon insurance. This means that our wide range of substance abuse treatment programs are accessible to those who need them.
We are dedicated to providing you with the highest quality of personalized care. We use a mix of proven methods and whole-body therapies to help you heal and set you up for a lasting recovery.
Here we explain Carelon’s coverage and show you our programs. Together, we will work to create a healthier future for you, free from substance abuse!
Jump to the following sections
View our addiction treatment locations
Now Accepting AHCCCS Health Choice,
Mercy Care, TriCare, and Triwest
Addictions we treat at Cornerstone
CARELON COVERED DRUG REHAB PROGRAMS

Our Residential Treatment Programs are designed to provide comprehensive and continuous support for individuals struggling with substance abuse. Integrating detoxification, counseling, and holistic recovery methods creates a nurturing environment for healing. Our treatments are rooted in proven methodologies, including Cognitive-Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT), enriched with mindfulness practices, yoga, and nutrition education. We aim to help individuals address the underlying factors of their addiction, equipping them with essential tools for lasting recovery and relapse prevention.

Our Partial Hospitalization Programs (PHP) for substance abuse are structured to provide a comprehensive journey toward recovery. These programs operate five days a week, six hours daily, offering intensive daytime care that includes therapy, group activities, and holistic approaches. This format enables individuals to address and manage their addiction challenges while also gaining vital skills and support necessary for maintaining prolonged sobriety. By promoting accountability and encouraging the application of acquired strategies in real-life situations, our PHP supports individuals in achieving lasting recovery.

Our Intensive Outpatient Program (IOP) is the gateway to aftercare, providing clients with the extra support needed before beginning their new life after treatment. We have several outpatient programs to choose from which operate 3, 4, and 5 days a week with adaptable scheduling to accommodate individual commitments and responsibilities. We also offer supportive housing. These programs feature a variety of therapeutic approaches, including personalized counseling, group therapy, and workshops aimed at developing skills. With a comprehensive and caring approach, we facilitate a path to recovery and rebuilding lives affected by addiction, emphasizing a holistic and supportive strategy throughout the journey.
Carelon Health Insurance
Carelon Health Insurance specializes in providing insurance solutions to meet the diverse needs of its members. Founded to address the evolving healthcare landscape, Carelon offers comprehensive coverage, including preventive care, emergency services, and specialized treatments like substance abuse rehabilitation.1 Carelon is committed to enhancing the health and well-being of its members, and its focus on innovation and service in the health insurance sector ensures access to quality care and support for individuals and families.
ABOUT CARELON DRUG TREATMENT COVERAGE
Carelon Insurance is committed to supporting individuals who are on their path to recovery from substance abuse. They specialize in providing coverage for essential services like inpatient and outpatient rehabilitation programs, therapy sessions, detoxification, and ongoing support mechanisms.2 This insurance company offers a wide range of treatment options to meet the diverse needs of those seeking help. They provide access to personalized treatment plans that leverage evidence-based practices and holistic approaches to foster sustainable recovery and well-being. Carelon’s commitment to providing comprehensive care is evident in the various programs it covers.
Alumni Client Family Testimonial
“I feel like Cornerstone gave him all the right tools. He knew how to do it. It was something we could have never done. I just could totally see kind of a personality change in him of wanting, and knowing, that he could achieve and do higher things and greater things. That has to be the people [at Cornerstone]”.
Nicole A. - Mother of a Cornerstone Alumni
What Addictions Does Carelon Provide Coverage For?
Addictions Covered by Carelon
Carelon insurance plans provide extensive coverage for managing substance abuse disorders, covering alcohol and drug rehab services. Below are addiction treatments available at our Arizona facilities, potentially included in your health insurance coverage:
- Alcohol: Comprehensive support for overcoming alcohol addiction is provided by Carelon insurance.
- Opioids: Carelon plans offer full care and assistance for individuals overcoming opioid addiction.
- Fentanyl: Treatment for fentanyl addiction, complete with specialized care and support, is included in Carelon insurance.
- Cocaine: Carelon covers tailored treatment strategies designed to combat cocaine addiction and support sustained sobriety.
- Methamphetamine: Addressing the underlying issues of meth addiction is supported, ensuring effective recovery through Carelon insurance.
- Benzodiazepine: Withdrawal and rehabilitation treatments for benzodiazepine dependency are covered under Carelon plans.
- Co-Occurring Disorders: Individuals with dual diagnoses of addiction and mental health conditions receive customized therapy, covered by Carelon insurance.
Programs We Offer
UNDERSTANDING YOUR CARD AND USING YOUR BENEFITS
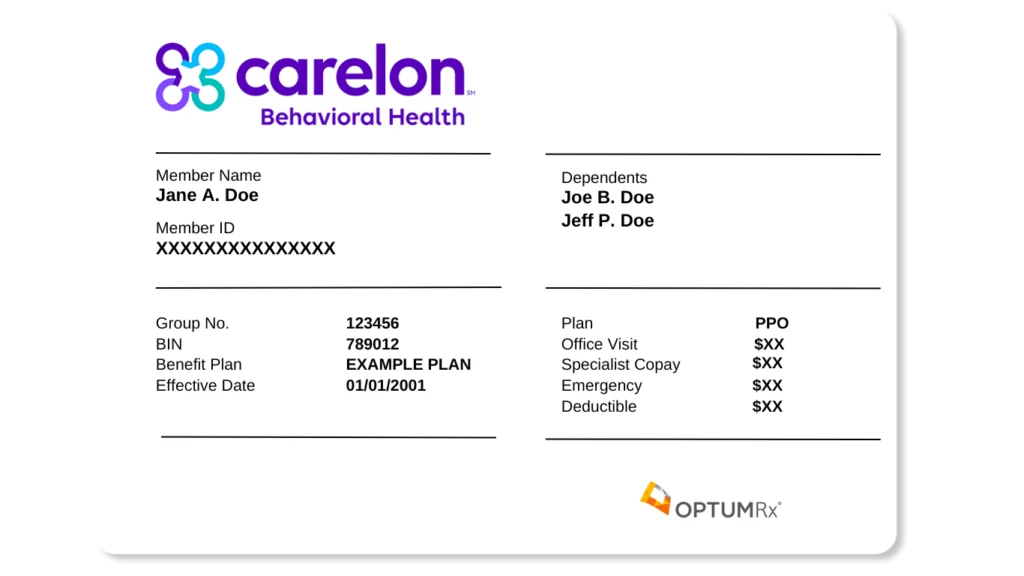
Card Front
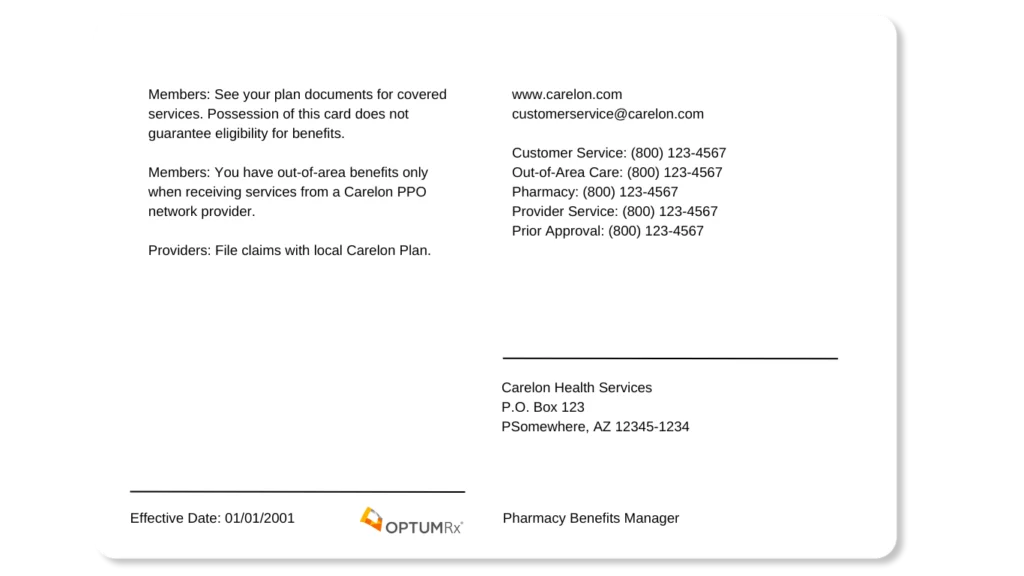
Card Back
MEET OUR CLINICAL TEAM

Clinical Director of Scottsdale Program
Lionel is a Licensed Independent Substance Abuse Counselor (LISAC) with over 4 years at Cornerstone. Passionate about helping those with addiction and mental health struggles, and he has trained as an EMDR therapist, adopting a trauma-informed approach to find and treat underlying root causes with empathy.

Clinical Director of Phoenix Program
Nate began his recovery journey in 2010 and earned a Master’s in Social Work from ASU. He’s been in the Behavioral Health field since 2013. Specializing in CBT, DBT, and grief, Nate is now the Clinical Director of our Phoenix program, underlined by his passion for helping others who struggled with substance abuse issues as he did.
FAQs About Carelon Health
Substance Abuse Treatment Coverage
Get answers to the most commonly asked questions about utilizing Carelon drug rehab coverage for substance abuse treatment.
What types of drug rehab programs does Carelon cover?
Carelon health insurance offers a variety of services for addiction treatment, with coverage details dependent on your specific plan and geographic location.
Coverage often includes:
- Detoxification: Assistance during detox to help safely manage withdrawal symptoms.3
- Inpatient Rehabilitation: Provides therapy, medical care, and support within a residential setting.
- Outpatient Rehabilitation: Enables treatment while living at home, incorporating therapy and group meetings.
- Partial Hospitalization Programs (PHP): Offers intensive treatment on a daily basis, serving as an intermediary step between inpatient and outpatient care.
- Intensive Outpatient Programs (IOP): A less intensive option than PHP, focusing on recovery skills and therapy for a few hours each day.
- Counseling and Therapy: Access to individual, group, and family sessions to tackle the behavioral challenges of addiction.
Reviewing your Carelon insurance benefits is essential to understand the coverage for different treatment options, including any limitations or prerequisites, and how to utilize these services effectively.
If you need help, our Cornerstone team understands insurance policies and can immediately begin reviewing your benefits once you verify your insurance with us!
Will Carelon cover my stay in rehab?
Carelon generally provides coverage for addiction treatment stays, although coverage details, including scope and specifics, can differ widely based on your policy, required treatment type, and other considerations.
Key aspects to know about your coverage include:
- Treatment Types: Carelon supports both inpatient and outpatient treatments. This includes detoxification, residential care, and necessary medical treatments for inpatient services. Outpatient services cover therapy sessions, group counseling, and partial hospitalization programs.
- Pre-Authorization Requirement: Often, treatments require pre-authorization from Carelon, meaning approval is needed before starting treatment to ensure coverage.
- Choosing Providers: Utilizing in-network providers typically ensures maximum coverage under Carelon, as they have a network of preferred providers. Services from out-of-network providers may be covered but often at a different rate, depending on your plan’s specifics.
- Understanding Deductibles and Co-pays: It is vital to know your deductibles and co-pays, as these will influence your treatment’s out-of-pocket costs.
- Coverage Duration: The coverage for the length of inpatient stays or the number of outpatient sessions varies by policy.
- Type of Addiction: The substance or behavior you’re receiving treatment for may affect coverage, with certain plans having specific conditions or exclusions for different types of addiction.
- Ongoing Treatment Review: The need for continued treatment will be regularly assessed to confirm its medical necessity, impacting the length of coverage for your treatment.
Understanding these elements can help you better understand your Carelon insurance coverage for addiction treatment.
It’s advisable to review your policy thoroughly or consult with a healthcare professional to help you navigate and understand your specific coverage details.
At Cornerstone, we can help you determine your benefits by verifying your insurance coverage and eliminating any uncertainties regarding what is and isn’t covered.
How long will Carelon cover my stay in rehab?
The duration of substance abuse rehabilitation coverage by Carelon can differ and be influenced by your policy details, required treatment type, and personal needs.
Essential points include:
- Policy Terms: The coverage period varies across Carelon plans. While some policies specify a certain number of days annually for inpatient care, others may limit the number of covered outpatient sessions.
- Medical Necessity Basis: Coverage hinges on the treatment’s medical necessity. Carelon is more inclined to cover treatments viewed as necessary and fitting for your case, subject to ongoing evaluations and assessments throughout the treatment.
- Inpatient and Outpatient Differences: Typically, inpatient treatments (residential stays) are covered for a shorter period compared to outpatient treatments (treatment sessions while living at home), with inpatient coverage ranging from a few weeks to about a month and outpatient potentially extending for a longer duration based on session intensity and frequency.
- Ongoing Treatment Evaluation: The need for continued treatment is regularly reviewed. Coverage continues up to the plan’s specified limits as long as the treatment remains medically necessary and progress is evident.
- Understanding Policy Limits: Familiarize yourself with any annual or lifetime limits in your policy, as these may restrict the number of days or sessions covered within a specific timeframe.4
If you want to know how long your Carelon policy covers rehabilitation, it’s recommended that you review your policy details or speak to a healthcare provider or Carelon representative.
They can give you information on the coverage that suits your treatment needs and situation.
Will Carelon pay for rehab more than once?
Carelon provides coverage for multiple addiction treatments, although this is contingent upon your policy’s specific provisions, limitations, and exclusions, as well as the medical necessity and outcomes of any previous treatments.
Here are the key factors to consider:
- Annual and Lifetime Caps: Some policies may limit the frequency of treatment for substance abuse within a given year or over the policy’s lifetime. Reviewing your plan for any stated restrictions on the number of treatment episodes or covered days is important.
- Medical Necessity: Carelon typically requires a determination of medical necessity for each treatment episode, meaning a healthcare professional must attest to the treatment’s critical nature for your recovery.5
- Outcome of Prior Treatment: The decision to cover additional treatment sessions will often consider the effectiveness and progress of any prior treatment, focusing on the necessity and potential benefits of further treatment.
- Treatment Modality: The type of treatment you’re seeking affects coverage; for example, Carelon might cover a series of outpatient therapy sessions annually more consistently than it does multiple inpatient rehab stays.
- Specific Policy Details: Understanding the nuances of your particular Carelon plan is essential, as policies differ significantly in their approach to covering repeated treatments.
- Pre-Authorization Requirement: ust like initial treatments, subsequent treatments usually need pre-authorization from Carelon to ensure they are eligible for coverage and deemed medically necessary.
To navigate coverage for addiction treatments, review your Carelon policy, contact Cornerstone to verify your insurance benefits, or consult a Carelon representative to clarify repeated treatment coverage.
Are there any restrictions on types of addiction treatment Carelon will pay for?
Like other insurers, Carelon imposes specific restrictions or limitations on the addiction treatments it covers based on criteria such as medical necessity, evidence-based efficacy, cost-effectiveness, and the particulars of your insurance plan.
Common limitations may involve:
- Type of Treatment: Coverage might be limited to certain treatment modalities, such as inpatient, outpatient, or medication-assisted therapy (MAT), excluding luxury or experimental approaches.
- Network of Providers: Carelon maintains a network of approved addiction treatment providers. Seeking treatment outside this network could increase personal costs or cause a lack of coverage.
- Pre-Authorization Requirement: Many Carelon plans mandate pre-authorization for addiction treatments, necessitating prior approval to confirm coverage.6
- Duration and Frequency of Treatment: There may be caps on the length and frequency of treatments, such as a set number of inpatient days or therapy sessions.
- Substance-Specific Coverage: Coverage can vary depending on the substance being treated, and certain drugs or behaviors can potentially be excluded or limited.
- Evidence-Based Treatments: Carelon typically covers only treatments with proven effectiveness based on scientific evidence.
- Appropriate Level of Care: Coverage is extended only to the level of care assessed as necessary for the patient’s condition, potentially limiting access to more intensive treatments unless medically justified.
Understanding the scope of your coverage involves navigating numerous factors.
Please get in touch with our admissions team for personalized guidance based on your specific situation.
How soon can I get into rehab with Carelon coverage?
The timeframe for initiating treatment may differ, but at Cornerstone Healing Center, our goal is to facilitate a quick and seamless entry into our program.
Starting the admissions process and reserving your spot in our facility is straightforward when you contact us directly.
Our committed team is on hand to assess your requirements, confirm your Carelon insurance benefits, and manage your admission details.
We aim to support you at every stage, ensuring you can embark on your path to recovery without delay.
Sources
CLINICALLY REVIEWED

Lionel Estrada, LISAC
CLINICAL DIRECTOR
Lionel, a Licensed Independent Substance Abuse Counselor (LISAC) with over 4 years at Cornerstone, specializes in addiction and mental health. Trained in EMDR therapy, he employs a trauma-informed, empathetic approach to address underlying causes of these issues.
- Read our Editorial Policy
Still have questions about treatment?
Our admissions specialists are here to explain the process, answer any questions you may have, and ensure you’re getting the help you need to live a healthy life free from addiction.






















